Direct Fluorescent Antibody (DFA) Technique best 2024: A Critical Tool in Diagnostic Microbiology
Introduction
The direct fluorescent antibody (DFA) technique is a cornerstone in diagnostic microbiology, providing a rapid and specific method for detecting pathogens in clinical samples. This technique leverages the specificity of antibodies and the visibility of fluorescent dyes to identify microorganisms directly in patient samples, bypassing the need for culture growth. The DFA method has become indispensable in various medical and research applications, particularly in diagnosing infectious diseases, where time is often of the essence. This article explores the principles, applications, advantages, and limitations of the direct fluorescent antibody technique, emphasizing its critical role in modern diagnostics.
Principles of direct fluorescent antibody Technique
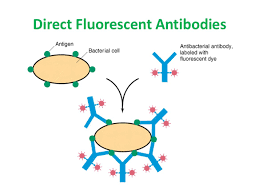
The DFA technique is based on the use of antibodies labeled with fluorescent dyes. These antibodies are designed to bind specifically to antigens, which are typically proteins or polysaccharides on the surface of pathogens. When a sample containing the target pathogen is treated with these fluorescently labeled antibodies, the antibodies bind to the antigens, forming an antigen-antibody complex. Under a fluorescent microscope, the presence of these complexes can be visualized as bright spots of fluorescence, indicating the presence of the pathogen.
The success of the DFA technique hinges on the specificity of the antibodies used. These antibodies must bind only to the target pathogen without cross-reacting with other microorganisms or host cells. This specificity is achieved through careful selection and production of monoclonal or polyclonal antibodies that are tailored to recognize unique antigens associated with the pathogen of interest.
Applications of direct fluorescent antibody in Diagnostic Microbiology
The direct fluorescent antibody technique is widely used in clinical diagnostics due to its ability to provide rapid and accurate results. Some of the key applications include:
1. Respiratory Infections
One of the most common uses of DFA is in the diagnosis of respiratory infections, particularly those caused by viruses such as Influenza A and B, Respiratory Syncytial Virus (RSV), and Parainfluenza viruses. These viruses are significant causes of morbidity and mortality, especially in vulnerable populations like infants, the elderly, and immunocompromised individuals. The DFA technique allows for the direct detection of these viruses in respiratory secretions, such as nasopharyngeal swabs or aspirates, within hours. This rapid turnaround is crucial in guiding timely antiviral therapy and infection control measures.
2. Sexually Transmitted Infections (STIs)
DFA is also employed in the detection of sexually transmitted infections, particularly in identifying pathogens such as Treponema pallidum, the causative agent of syphilis. Treponema pallidum is difficult to culture, making DFA one of the preferred methods for direct detection. The DFA technique can identify the organism in clinical specimens such as lesion exudates, providing a quick diagnosis that is essential for effective treatment and prevention of transmission.
3. Parasitic Infections
In parasitology, DFA is used to detect parasites like Cryptosporidium and Giardia in stool samples. These parasites are common causes of gastrointestinal illness, particularly in immunocompromised patients and in outbreaks associated with contaminated water. The DFA method is highly sensitive and specific, making it a valuable tool in both clinical diagnosis and public health investigations.
4. Rabies Diagnosis
Rabies, a fatal viral encephalitis, is diagnosed using the DFA technique in brain tissue samples from suspected animals or humans. The rapid and accurate identification of the rabies virus using DFA is vital in deciding the course of treatment and in public health responses to potential rabies exposures.
Advantages of the DFA Technique
The DFA technique offers several advantages that make it a preferred method in various diagnostic settings:
1. Speed
One of the primary advantages of DFA is its rapid turnaround time. Unlike culture-based methods, which can take days to weeks, DFA can provide results within hours. This speed is particularly important in the context of infectious diseases where early diagnosis can significantly influence treatment outcomes and prevent the spread of infection.
2. Specificity
The use of highly specific antibodies in DFA ensures that the technique has a high degree of specificity. This reduces the likelihood of false positives, providing confidence in the diagnostic results. The ability to tailor antibodies to recognize specific antigens also allows for the development of DFA assays for a wide range of pathogens.
3. Direct Detection
DFA allows for the direct detection of pathogens in clinical samples without the need for culture. This is particularly beneficial for pathogens that are difficult or slow to culture, or when the patient has already received antimicrobial therapy that might inhibit growth in culture.
4. Quantification
In some cases, DFA can provide semi-quantitative or quantitative information about the level of pathogen present in a sample. The intensity of fluorescence can be correlated with the concentration of the pathogen, providing useful information for assessing the severity of infection.
Limitations of the DFA Technique
Despite its advantages, the DFA technique has some limitations that must be considered:
1. Labor-Intensive
The DFA technique requires skilled personnel to perform the assay and interpret the results. The preparation of samples, the application of fluorescent antibodies, and the reading of slides under a fluorescence microscope are all tasks that require technical expertise. This can be a limiting factor in resource-limited settings where trained personnel may not be available.
2. Need for High-Quality Specimens
The accuracy of DFA is highly dependent on the quality of the specimen. Poorly collected or stored samples can lead to false-negative results. For example, in respiratory infections, improper collection of nasopharyngeal swabs can result in insufficient viral material, reducing the sensitivity of the test.
3. Cost
The cost of fluorescent antibodies and the specialized equipment required for DFA, such as fluorescence microscopes, can be prohibitive, particularly in low-resource settings. Additionally, the ongoing cost of reagents and maintenance of equipment adds to the overall expense of using DFA.
4. Limited Sensitivity
While DFA is generally highly specific, its sensitivity can be lower than that of nucleic acid-based methods, such as PCR (Polymerase Chain Reaction). DFA may not detect very low levels of pathogen, leading to false-negative results, especially in early stages of infection or in samples with low pathogen load.
Future Directions and Innovations
The DFA technique continues to evolve, with ongoing research aimed at improving its sensitivity, specificity, and ease of use. Some of the emerging innovations in this field include:
1. Multiplex DFA Assays
Multiplex DFA assays are being developed to detect multiple pathogens simultaneously in a single sample. This approach is particularly useful in respiratory infections where co-infections with multiple viruses or bacteria are common. Multiplex DFA can provide comprehensive diagnostic information rapidly, aiding in the management of complex infections.
2. Automated DFA Systems
Automation is being introduced into DFA workflows to reduce the labor-intensive nature of the technique. Automated systems can handle sample preparation, staining, and even image analysis, reducing the need for skilled personnel and improving throughput. This is particularly beneficial in high-volume laboratories.
3. Integration with Molecular Techniques
There is growing interest in integrating DFA with molecular techniques such as PCR. This hybrid approach can combine the strengths of both methods, offering the specificity and rapidity of direct fluorescent antibody with the sensitivity of molecular detection. Such integrations can enhance diagnostic accuracy, particularly in cases where low pathogen levels are a concern.
Conclusion
The direct fluorescent antibody (DFA) technique remains a vital tool in the diagnostic microbiology arsenal, offering a rapid and specific method for pathogen detection. Its applications in diagnosing respiratory infections, STIs, parasitic infections, and rabies underscore its versatility and importance in clinical diagnostics. However, the technique is not without its challenges, including the need for skilled personnel, high-quality specimens, and specialized equipment. As innovations continue to emerge, the direct fluorescent antibody technique is poised to become even more integral to the rapid diagnosis of infectious diseases, ultimately improving patient outcomes and public health responses.